By Michael Strøm

Choosing the suitable shockwave technology for your clinical setting is easy if you consider the following:
- What is your primary type of indication? Is it working with tissue or with cells? Or a combination of both?
- Is your clinic focused on basic or advanced indications?
- What direction do you want to grow your clinic? Do you want to work generally or very specifically?
- What type of financial investment are you willing to make?
General Approach and Basic Indications
Suppose you want to work with shockwave technology across various indications for tissue and tendons, and even some aesthetic indications. In that case, the radial shockwave device (also known as RSWT, radial pressure wave [properly known as] or acoustic wave) would be a good solution for your clinic.
RSW generates oscillations in the tissue, leading to improved microcirculation and increased metabolic activity, making quicker healing possible.
These effects are what make RSWT a perfect solution for working with myofascial conditions, both in regular indications or in conjunction with enhancing recovery in elite athletes.
When we look at some of the effects seen in RSWT, they can be listed as follows:
- Release of trigger points
- Stimulation of circulation
- Treatment of myofascial indications
- Tensile strength
- Lymphatic activity
- Tissue mobilization
In general, RSWT opens the possibility to efficiently treat many indications that affect people daily. These include common conditions; such as epicondylitis, plantar fasciitis, calcification in the shoulder, DOMS, and general trigger points.
The technology is easy to use and with proper training, you will have the foundation to work with basic indications safely. It is a great addition to the rehabilitation process, where it can reduce tension in muscles, reduce pain and increase the range of motion. These types of results generate a high amount of compliance and satisfaction with clients.
In addition, radial shockwave can be the first part of the path into more advanced application use later on. Begin with radial for basic applications at a lower price point and then grow into more advanced indications when pairing with a focused device later on.
Specific Approach and Advanced Indications with shockwave technology
If you want to work with more advanced indications and pair shockwave with many different types of therapy then the focused shockwave will be the right option. It could be tendinopathies, wound healing, calcifications, neuropathy, fractures, and even urology indications.
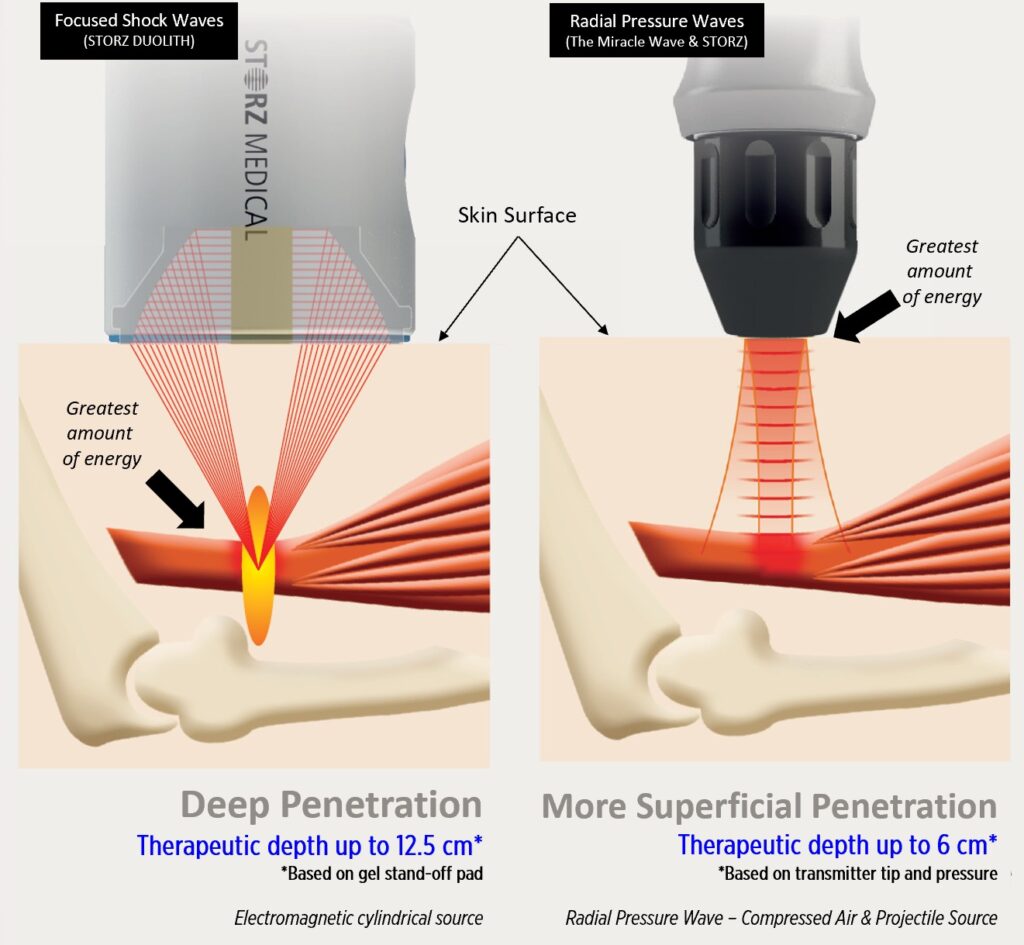
When we work with the focus shockwave technology, we can work more precisely in a focal area in comparison to the wider energy delivery in radial pressure waves. We work with stimulation of the cells with specific intensity (mJ/mm2) into a specific depth of the tissue we have decided. That makes it a potent tool in the toolbox of safe, noninvasive technologies.
One of the main factors of the focused shockwave is the biological effects associated with mechanotransduction. It explains the release of different biochemical substances, such as substance P (related to pain), growth factors, and nitric oxides (NO).
We also see that shockwave therapy results in increased blood circulation and metabolic activity stimulation, enhancing the healing process in different tissue types.
Some of the other effects we know from basic research include:
- Increase in cell permeability
- Stimulation of stem-cells
- Reduction of non-myelinated nerve fibers
- Antibacterial effect
- Stimulation of microcirculation
- Release of growth hormones
- Stimulation of neurons
Focused shockwave requires additional training in the initial phase, but when the basic training is complete, it pushes your clinic to grow to the next level, differentiating you from your competitors.
The focused units have a higher price point than the radial systems, as they give access to more advanced indications and higher turnaround in the clinic, leading to a more significant return on investment in the long run.
The Premium Option
If you want to offer your client a premium setup, better results are seen by combining the two different technologies. They enhance the effect of each other and will give you very few limitations in the various indications you would think of treating.
That is also why most of the leading experts in shockwaves globally do a combination of radial and focus shockwaves.
Summary
Look into which shockwave technology enhances your clinical setup and what you want to treat now and in the future. And otherwise, you can always reach out to our clinical experts to receive guidance on how shockwave can fit your specific needs and the growth of your clinic.
References
Cleveland, R. O. et al.: Acoustic field of a ballistic shock wave therapy device. Ultrasound in medicine and biology, 33(8), 1327 – 1335, 2007.
Grecco, M. V. et al.: One-year treatment follow-up of plantar fasciitis: radial shockwaves vs. conventional physiotherapy. Clinics, 68(8),1089 –1095, 2013.
Bloch. W., Suhr, F :mechanotransduction: mechanical stimulation of biological processes. How shock and pressure waves initiate the healing process. Multidisciplinary medical applications. Level10buchverlag, heilbronn, 2014: p. 50-69
Ulrich Dreisilker: ENTHESOPATHIES KNOWLEDGE UPDATE: Pressurewaves: mechanism of actions p. 42-44
(https://www.shockwavetherapy.org/about-eswt/shockwave-history/)(Wess, O. et al.: Working group technical developments – consensus report. In: Chaussy, C. et al. (eds.): High Energy Shock Waves in Medicine. Georg Thieme Verlag, Stuttgart, 1997.)
Maier, M. et al.: Substance P and prostaglandin E2 release after shock wave application to the rabbit femur. Clinical Orthopaedics and Related Research, (406), 237 – 245, 2003.
Mariotto, S. et al.: Extracorporeal shock waves: From lithotripsy to anti-inflammatory action by NO production. Nitric Oxide, 12(2), 89 – 96, 2005.
Byron, C. R. et al.: Effects of radial shock waves on membrane permeability and viability of chondrocytes and structure of articular cartilage in equine cartilage explants. American Journal of Veterinary Research, 66(10), 1757 – 1763, 2005.
Schuh, C. M. et al.: In vitro extracorporeal shock wave treatment enhances stemness and preserve multipotency of rat and human adipose-derived stem cells. Cytotherapy, 16(12), 1666 – 1678, 2014.
Raabe, O. et al.: Effect of extracorporeal shock wave on proliferation and differentiation of equine adipose tissue-derived mesenchymal stem cells in vitro. American Journal of Stem Cells, 2(1), 62 – 73, 2013.
Klonschinski, T. et al.: Application of local anesthesia inhibits effects of low-energy extracorporeal shock wave treatment (ESWT) on nociceptors. Pain Medicine, 12(10), 1532 – 1537, 2011.
Church, C.: A theoretical study of cavitation generated by an extracorporeal shock wave lithotripter. The Journal of the Acoustical Society of America, 86(1), 215 – 227, 1989.
Kisch, T. et al.: Repetitive shock wave therapy improves muscular microcirculation. Journal of Surgical Research, 201(2), 440 – 445, 2016.
Goertz, O. et al.: Short-term effects of extracorporeal shock waves on microcirculation. Journal of Surgical Research, 194(1), 304 – 311, 2015.
Nishida, T. et al.: Extracorporeal cardiac shock wave therapy markedly ameliorates ischemia-induced myocardial dysfunction in pigs in vivo. Circulation, 110(19), 3055 – 3061, 2004.
Chao, Y.-H. et al.: Effects of shock waves on tenocyte proliferation and extracellular matrix metabolism. Ultrasound in medicine and biology, 34(5), 841 – 852, 2008.
Christ, Ch. et al.: Improvement in skin elasticity in the treatment of cellulite and connective tissue weakness by means of extracorporeal pulse activation therapy. Aesthetic Surgery Journal, 28(5), 538 – 544, 2008.
Gollwitzer, H. et al.: Radial extracorporeal shock wave therapy (rESWT) induces new bone formation in vivo: results of an animal study in rabbits. Ultrasound in medicine and biology, 39(1), 126 – 133, 2013.
Wess, O.: A neural model for chronic pain and pain relief by extracorporeal shock wave treatment. Urological Research, 2008; 36(6), 327 – 334, 2008.
Beisteiner, R. et al.: Transcranial Pulse Stimulation with Ultrasound in Alzheimer’s Disease – A New Navigated Focal Brain Therapy. Advanced Science, 7(3):1902583, 2019. doi: 10.1002/advs.201902583.
